Eliminating Central Line–Associated Bloodstream Infections: Is It Possible? - Medscape
Hospital-acquired infections (HAIs) are a very serious matter; thousands of patients die each year as a result, and healthcare facilities expend tremendous resources aimed at prevention.[1] Central line—associated bloodstream infections (CLABSIs), in particular, are a vexing and seemingly intractable problem. This HAI has been estimated to cost nearly $2 billion annually with an estimated mortality of 16%.[2] However, only an estimated 65%-70% of CLABSIs are considered reasonably preventable by using evidence-based strategies.[3] An update on these strategies was recently published that provides additional guidance addressing the issue.[4]
The National Healthcare Safety Network (NHSN), a division of the Centers for Disease Control and Prevention (CDC), publishes and updates yearly the complex HAI surveillance definitions that each participating hospital is required to follow.[5] Infection prevention staff apply these stringent definitions to their daily surveillance in order to accurately report all such HAIs into the NHSN database. Each hospital's standardized HAI rates are publicly reported by the Centers for Medicare & Medicaid Services and serve as quality measures in its Value-Based Purchasing Program.
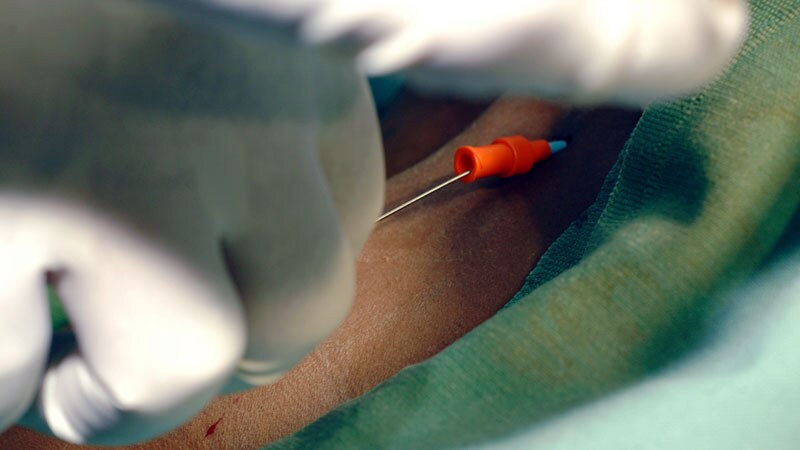
It's important to understand the definitions used in this context. A catheter-related bloodstream infection (CRBSI) is a serious hospital-acquired condition that can lead to sepsis, excess length of stay, and death. According to the CDC's website (emphasis is the author's)[6]:
CRBSI is a clinical definition, used when diagnosing and treating patients, that requires specific laboratory testing that more thoroughly identifies the catheter as the source of the BSI [bloodstream infection]. It is not typically used for surveillance purposes. Simpler definitions are often used for surveillance purposes. For example, CLABSI is a term used by CDC's National Healthcare Safety Network (NHSN)…. A CLABSI is a primary BSI in a patient that had a central line within the 48-hour period before the development of the BSI and is not bloodstream related to an infection at another site. However, since some BSIs are secondary to other sources other than the central line (e.g., pancreatitis, mucositis) that may not be easily recognized, the CLABSI surveillance definition may overestimate the true incidence of CRBSI.
The CLABSI definition is a highly sensitive, nonspecific, simplistic surveillance definition that is intended to capture all bloodstream infections in any hospitalized patient with a central venous catheter (CVC) — for example, a peripherally inserted central catheter, accessed port, triple-lumen CVC, or hemodialysis catheter. The catheter must be in place for at least 2 calendar days, with the date of insertion being calendar day 1. For the purposes of reporting to NHSN, the source of the blood culture (drawn from a catheter or peripherally) is irrelevant. Furthermore, blood culture isolates that are not considered commensals (eg, Staphylococcus aureus, Klebsiella species, Candida species) do not require clinical parameters (eg, fever, leukocytosis, hypotension) to be reportable as a CLABSI.[6]
For example, a patient had a CVC placed for total parenteral nutrition. Five calendar days later, her white blood cell (WBC) count increased from 10,000 to 15,000, but the patient was otherwise doing well — specifically, without fever or systemic symptoms. The concerned physician ordered blood cultures because of the increase in WBC count. Samples for culture were obtained both peripherally and via the CVC. Two days later the WBC count normalized, but blood culture of the sample obtained through the CVC revealed Candida albicans. The peripheral blood culture was negative. The patient was clinically well. Although clinically interpreted as a contaminant, because of the clinical scenario and because only the CVC culture yielded growth, this scenario nonetheless fulfills criteria as a CLABSI and is reportable to NHSN.
Even in patients with fever or evidence of sepsis, a CLABSI may still not be a true CRBSI in the clinical sense; some microbial isolates might be contaminants, whereas others might represent transient bacteremias from other sources, such as the gastrointestinal tract in chronically ill patients (eg, those with advanced gastrointestinal tract cancer or enteral nutrition–depleted patients incurring prolonged hospitalizations).[7,8]
Given this situation, how can a hospital's medical staff help to reduce its reported CLABSI rate?
Be extremely judicious when considering a CVC in the first place. My facility created the mnemonic PITCH for appropriate indications: Parenteral nutrition, Inotropes or vasopressors, Transvenous pacing, Cancer chemotherapy, and Hemodialysis or hypertonic saline.
Use insertion checklists for all CVCs.
Early enteral nutrition should be the goal in all critically ill patients because it reduces overall risk for infection. Total parenteral nutrition should be reserved for when there is an absolute contraindication to using the gut as the primary source of caloric delivery.[9]
Remove the CVC as soon as the original indication is resolved. Poor intravenous access and need for blood draws are not acceptable reasons.
Be judicious when ordering blood cultures.
Regarding the latter, it is extraordinarily difficult in the real world to stratify the pretest probability of a bloodstream infection at the bedside of a critically ill patient with a CVC.[10] However, although CLABSIs may not be as amenable to diagnostic stewardship as Clostridioides difficile and catheter-associated urinary tract infections, there are opportunities for improvement: Develop a consensus for not ordering blood cultures in low-likelihood situations, such as an elevated WBC count without other evidence of systemic infection.[11,12] This could and should be part of a larger strategy to minimize all unnecessary blood work across the institution, such as serial complete blood cell counts and basic metabolic panels. This has the potential to improve patient satisfaction and reduce costs.[13]
I hope this brief overview adequately portrays the problem at hand. Only by pooling collective expertise and working as a team with a shared common goal will it be possible to achieve sustainable reductions not just for CLABSIs but also for other hospital-acquired infections (eg, catheter associated urinary tract infections). Although we all strive for zero HAIs, in the context discussed in this article, this may not be realistically possible for CLABSIs.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube

Comments
Post a Comment